The beginning of wisdom is to call things by their right names
In this blog I reflect upon my mental health diagnosis'; and the recent revelation that I am not a 'little bit bipolar' any more – and perhaps I never was? How I feel now that my 'confirmed' diagnosis is emotionally unstable personality disorder/ borderline personality disorder (EUPD/BPD) and what that means to me. I hadn't intended to publish it on World Mental Health Day but I think its timely that it is. It may be triggering...
In my ‘first ever’ blog I touched upon being informed in my appointment with a psychiatrist (I can’t say ‘my’ psychiatrist given that we will probably only have another 1 or 2 meetings plus we aren’t in America) that my diagnosis of cyclothymia had gone in the bin in 2016, replaced with emotionally unstable personality disorder (EUPD). EUPD is also known as borderline personality disorder (BPD) and borderline personality disorder is known in the World Health Organisation classification (ICD-10) as Emotionally unstable personality disorder, borderline type – and be careful not to mix it up with bipolar disorder which is also frequently referred to as BPD... - and they say we are the ones with the problem!? I will refer to it interchangeably throughout.
The psychiatrist explained to me that the symptoms of low mood, suicidal ideation and depression that I was currently experiencing, and the reason that I had sought help, were in the context of emotional dysregulation, (and that kind of made sense, in a way that it wouldn't have if my diagnosis was cyclothymia and EUPD or just cyclothymia alone). He explained that whilst my medications could and would be increased, and I could be prescribed a sedative, this was likely to be futile, only effective in managing short term risk. That what I really needed was long term intensive therapy.
You may think that being a nurse, a psychiatric nurse none the less, I would have worked out three years ago that one diagnosis had replaced the other, but up until recently, I believed that I had cyclothymia AND EUPD. To be fair, EUPD was a diagnosis I received in the post, on a discharge letter and the treatment offered to me (medication) remained the same. As well as an antidepressant, I take lamotrogine; its indications being among others, monotherapy or adjunctive therapy for bipolar disorder, and cyclothymia is described as a lesser form of this. So perhaps you can forgive me for my ignorance.
Yet with my EDNOS (Eating Disorder Not Otherwise Specified) I didn’t need someone to make it explicitly clear that I no longer met the criteria for a diagnosis; I have a healthy relationship with food, mainly since embarking on the seefood diet; I see food I eat it, I maintain a consistent weight, and have a fairly reasonable relationship with my body, I have done so for some years; albeit I self harm ocassionally. It is the same with depression; when I no longer feel depressed, I have more energy, feel less ‘sad’, make plans for the future, start enjoying things again, it is kind of obvious that I am no longer depressed. I haven’t needed anyone to be explicit, and I have been content to lose the symptoms, and diagnosis’. So why don’t I feel the same way about cyclothymia?
On reflection, I think it’s less about cyclothymia and more about EUPD. And less about EUPD and more about how the evidence and my experience are two very different things.
According to the ICD-10 emotionally unstable personality disorder is: A personality disorder in which there is a marked tendency to act impulsively without consideration of the consequences, together with affective instability. The ability to plan ahead may be minimal, and outbursts of intense anger may often lead to violence or “behavioural explosions”; these are easily precipitated when impulsive acts are criticised or thwarted by others. Two variants of this personality disorder are specified, and both share this general theme of impulsiveness and lack of self-control. F60.30 Impulsive type: The predominant characteristics are emotional instability and lack of impulse control. Outbursts of violence or threatening behaviour are common, particularly in response to criticism by others. F60.31 Borderline type: Several of the characteristics of emotional instability are present; in addition, the patient’s own self-image, aims, and internal preferences (including sexual) are often unclear or disturbed. There are usually chronic feelings of emptiness. A liability to become involved in intense and unstable relationships may cause repeated emotional crises and may be associated with excessive efforts to avoid abandonment and a series of suicidal threats or acts of self-harm (although these may occur without obvious precipitants).
The above can be reduced to 9 symptoms all of which feel very personal and judgemental; Fear of abandonment. Unstable relationships unclear or shifting self-image. Impulsive, self-destructive behaviors. Self-harm. Extreme emotional swings. Chronic feelings of emptiness. Explosive anger.
How can I be RCNi Mental Health Nurse of the Year and I have all of these things!? How can I even function!?
In the absence of any conversation with a professional, other than the recent assessment, I have been having that conversation with myself, and what EUPD means to me...
I can identify with the descriptions that relate to self; self image, self destruction, self harm, mood swings, feelings of emptiness. The impulsivity, perhaps, if getting a tattoo, a piercing, or deciding to write a blog count as being impulsive, but in general, I am not so sure. Most of the things I do on impulse are to the benefit and certainly not the harm of others. Intense unstable relationships? I wouldn’t say so. Threats of self harm to avoid abandonment? Even when I should have sought medical help, I rarely have done so (not that I advise anyone else to do the same). Definitely not cries for attention, or efforts at being manipulative. But instead, for me unhelpful strategies to cope with internal pain.
Fear of abandonment? As according to a friend and something that I don’t dispute, I actively seek opportunities to be alone. I can identify with Dr. Perry D. Hoffman, of the National Education Alliance for Borderline Personality Disorder when he says “Unlike other psychiatric diagnoses, if you put someone with schizophrenia on an island all by themselves, their mental illness would still be evident. If you put someone with BPD on an island, you wouldn’t necessarily see the symptoms” This makes sense, because my workplace, my role as a nurse, that is my island, that is where I thrive and whereby my difficulties on the whole disappear… although the Hoffman does go on to say “whatever happens, happens in the context of [interacting] with someone else.” So maybe not.
Explosive anger? violence? Definitely not. I take pride in my ability to de-escalate most situations, both on the ward and off of it; it is not my stature that made me a successful ‘bouncer’ prior to embarking on my nurse training. I may have destroyed one or two pieces of crockery in my lifetime but who hasn't? AND, for the record, people with BPD are no more violent than the general population.
So in short, I can identify with some of the characteristics and not others. I can accept the diagnosis, even with the stigma attached to it. So that can’t be the problem.
And this is where my reflections start to head toward my conclusions. It is not about a diagnosis of EUPD at all, it is about the treatment or more precisely, the lack of it that has been available to me, and many others with the same diagnosis. The National Institute of Clinical Excellence even recognises this, with its guidance on the condition sharing my bleak prognosis and experience; “People with borderline personality disorder have sometimes been excluded from any health or social care services because of their diagnosis. This may be because staff lack the confidence and skills to work with this group of people.”
This guidance was produced in 2009, ten years later it has not been updated, and the reality is that that is because nothing has changed. Yet BPD need not be the hopeless, helpless condition that it was once thought to be, since the 1970s a 'revolutionary' treatment called dialectical behavior therapy; a “philosophic exercise in which two opposing views are discussed until a logical blending or balance of the two extremes — the middle way — is found" has been in existance. And that makes me angry because I have never been offered DBT.
What is more, according to NICE "You should not usually be offered medication specifically to treat borderline personality disorder or for any related symptoms or behaviour". So basically for three years, I have been given a 'band aid for a bullet wound' and not even an effective one at that. And what about the decade of medication that I have taken before that?
If as a professional (albeit a student nurse) at the time, I did not realise that one diagnosis had replaced the other, or that I should have had the expectation, or demanded that my treatment would change accordingly, how do we expect our patients, without the , to know?
And I feel rejected. I feel rejected because I self referred to IAPT earlier this year, but instead of a 6 week wait, after a lengthy assessment, and agreement that I would be eligible for compassion focused therapy, I was told that I was actually ‘too complex’. Instead I was offered a 4 months wait for triage, 6 months for an assessment, 12-24 months for therapy to start, with a generic service. And then I missed the assessment - feelings of emptiness and worthlessness got the better of me that day, I decided that the appointment should go to someone more deserving that me. And the response? I can not be re-referred for another 12 months as I have not showed willingness to engage or to change. (Nothing about the many phone calls I made to the service ahead of the assessment, expressing my desire to be seen before it reached crisis point).
My local mental health trust have a specific personality disorder service, and offers dialectical behavioural therapy (recommended by NICE guidelines), cognitive behavioural therapy (CBT), and motivational interviewing ‘based on the needs of the individual’. In the 3 years that I have had this diagnosis confirmed I have not been offered an assessment with said personality disorder service. Research has shown that 75% of those with borderline personality disorder treated with DBT improve after a year, and 95% of patients improved after two years. Yet I can not get the one thing that may help me.
I and 1% of the population have a psychiatric disorder, one that needs and can respond to treatment. Instead, for all too many, the only option available is medication, or crisis based admissions that can exacerbate the condition, or inflict further trauma on the already traumatised. 8% to 10% of BPD patients will commit suicide, we have an illness that without treatment may kill us. Yet we do not get the treatment that may save us. This World Mental Health Day is about suicide prevention. If in the future, I, and countless more people with my diagnosis shall become a statistic, please don’t say that we should have asked for help.
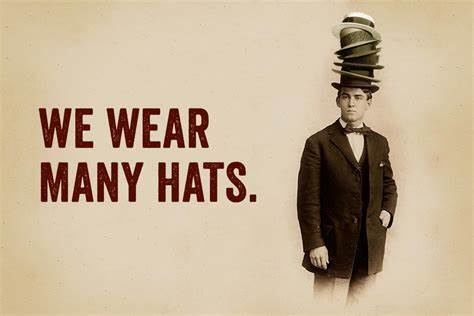
But then I put my nurse hat on. And I realise that the problem is not with me. The problem is that my mine and other’s reasonable responses; anger fear of abandonment, feelings of rejection, intense unstable relationships are seen as further evidence of the presense of symptoms, not inadequacies of services unable to cope with demand. Of a service and a system where so much of a psychiatrists time is taken up putting people into 'clusters'; meaningless to the individual but essential for currencies and payment, meeting c-quin targets or trying to discharge those in crisis back into the community, and from community services back into primary care that they are left with very little time for the 'patient'.
Comments
Post a Comment