It really is nothing like a broken leg!
'It's nothing like a broken leg': why I'm done with the mental health conversation’ @ladyhaja wrote for The Guardian in the Summer of 2018…
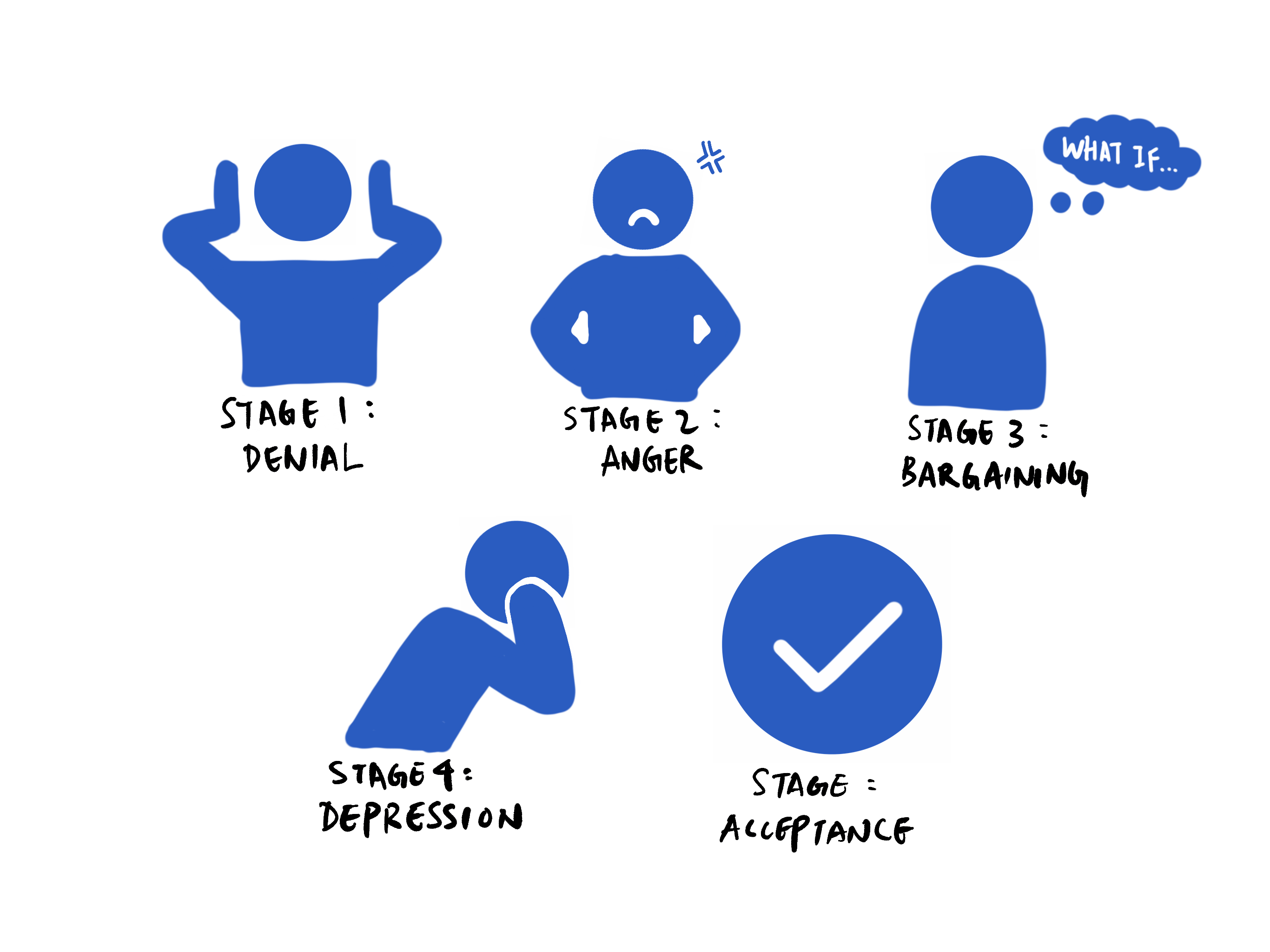
I have had this as the first lines of my ‘next blog’ for several weeks now. When I look back at what I had written after this, it makes me feel almost like a stranger, it’s almost humorous. I guess that was the denial stage. I then moved into anger and I couldn’t write for a while after that. I guess that month or so has been the bargaining and then the depression. (AGAIN!?)
I have come to think of my experience of mental health ‘services’ (or diservices) as a bereavement. It feels like a period of grief. I have moved from denial, (probably between age 19 to 31) to anger (that one has probably been the most damaging and started pretty much when I decided that I could no longer do it alone, I needed help), the bargaining, and now depression. It’s the acceptance that worries me, and comforts me the most.
When I started writing this some weeks ago, I was comparing my mental health experience to my ‘dislocated knee/ chipped femur’. I will do the same again, but make it briefer.
On Christmas Day 2018 I dislocated my knee. I have done it several times since, and several times before.
The NICE guidelines recommend:
“Management:
Provide adequate analgesia, arrange X-rays, immobilise in a cylinder cast POP (canvas back-splint for recurrent dislocation) and arrange orthopaedic follow-up.
Most clinicians suggest a short period of immobilisation (3-6 weeks) followed by rehabilitation with or without a patellar brace
Currently, there is no firm evidence that the natural history of the primary patellar dislocator is improved by acute surgical intervention, although after a second dislocation, repeat events become much more likely (49%) and surgery may be indicated.”
The second time that my knee dislocated, upon hearing that I was a mental health nurse, I was told ‘you work for the NHS, you are one of us. If you aren't cared for by us how can you care for your patients!?”. Within a week I had had an MRI, within four I had began physio, and I have seen the consultant orthopaedics regularly since. Each time my knee was immobilised. I was offered pain relief. On one occasion I had my knee drained; it meant the swelling would reduce. Each time I had follow up appointments. I am wearing something that resembles a donut but keeps my pattelar in place. It seems to work. For now. I have the option of surgery if it doesn't last. I have also been told that I have arthritis, and hypermobility; but given management plans for both.
 |
| This isn't actually me leg... unfortunately! |
Now let’s compare it to my mental health.
In January of this year, I set myself the target of getting ‘well’. I referred myself to IAPT (improving access to psychological therapies) when I was struggling. For the first time, I was honest. About how I felt, the trauma that I had experienced, the pain that I have carried around me since. It went well. I was offered compassion focused therapy. (I had CBT when I first was diagnosed with EDNOS, which was futile, and psychotherapy around 2012 which had helped, but I had not been ready to get to the root of my problems.)
Only shortly after I was told that I was too complex for IAPT. Instead I needed psychology. I have since realised that IAPT is a service subject to CQUINS and not wonder if it wasn't about my complexity but meeting targets instead. I started private therapy instead of wait for the 3 or so months for the assessment. Only I realised that it wasn't enough. I couldn't find one that offered MBT, DBT so I chose my therapist because I liked her name and I could afford her
| My therapist's name sounded lucky |
So I went to my GP, again I ripped myself open (metaphorically) I told her about the constant ‘nothingness’ the ‘emptiness’; the suicidality, the self harm - I don't self harm in the typical way, but for 2 reasons, 1 there is enough stigma around EUPD in itself to stigmatise myself further, especially when I am still in the 'active' phase, and 2 I don't believe in writing about 'methods'. She told me to go to A&E (I didn’t, I have been managing these feelings most days and I have never gone to A&E once), but she also referred me to psychiatry. She gave me a ‘life line’.
So again, I tore myself open, spoke about rape, decisions I made, how I have started to come to realise that my way of ‘taking back control’ was to punish myself, to re traumatise myself again and again and again. How therapy has helped me to realise that what I thought was normal, the small t’s of childhood, the big t’s of adulthood had shaped the way I feel and treat myself today. I explained that I am tired of this life. I am tired of hurting myself. I want to get better...
I was told that I don’t have cyclothymia anymore, I have a confirmed diagnosis of EUPD, I felt okay about that, he listened. He cared...
He also upped my medications. Which seemed odd, knowing that NICE guidelines state “Drug treatment should not be used specifically for borderline personality disorder or for the individual symptoms or behaviour associated with the disorder (for example, repeated self-harm, marked emotional instability, risk-taking behaviour and transient psychotic symptoms)” but I also found it validating. I knew I was in a dark place, that I needed something to help me see beyond the hole. To allow me to engage with the treatment that was indicated.
Surely now I had a ‘confirmed diagnosis’ I would get a personality disorder assessment, and the therapy I had been asking for… DBT, MBT, EDMR, anything. I could arrange my shifts around treatment. I was taking back control. All this pain, all the honesty. It was going to be worth it...
Or maybe not. Because he explained that he would have to ‘beg’ and I would have to ‘beg’ for psychology to reopen my case (because I didn’t keep that first appointment there was an entry on my notes saying not to re-refer for a year - punishment for disengaging (no one had asked me why).
I was hopeful. I looked at the NICE guidelines "consider a comprehensive dialectical behaviour therapy programme...When providing psychological treatment to people with borderline personality disorder as a specific intervention in their overall treatment and care, use the CPA to clarify the roles of different services, professionals providing psychological treatment and other healthcare professionals...When providing psychological treatment to people with borderline personality disorder, monitor the effect of treatment on a broad range of outcomes, including personal functioning, drug and alcohol use, self-harm, depression and the symptoms of borderline personality disorder.”
I was almost excited, I felt relief. This pain, the pain of being open and honest, making myself feel raw, it was going to be worth it. I was going to fill the cracks with gold. Like kintsukori. Only better.
Then the assessment with a psychologist happened...
And a month later I had heard nothing.
And so I phoned. And I phoned. And I phoned. Eventually I was told I had been discussed, and I was going to be offered CBT or psychoanalytic therapy; but first I had to be on a waiting list. Of approximately 2 years. I have no disrespect to those that work in the field (the private therapist I am seeing is trained in CBT) but I can't help but feel that if this didn't work aged 19, it's not likely to work now. I asked about a personality disorder assessment, or service, did I not meet the threshold "you work in mental health services, you know you don't".
So did I sink or swim? Did take back control... Off I went to the GP (again) asking for support with the co-morbidities. Thinking if perhaps I address them, I can start making progress with the private therapist. She told me it is not her field. I think she does not want to risk taking away my coping mechanism (however detrimental that may be). And also, the medication I am asking for is bloody expensive (I checked in the BNF)
So did I sink or swim? Did take back control... Off I went to the GP (again) asking for support with the co-morbidities. Thinking if perhaps I address them, I can start making progress with the private therapist. She told me it is not her field. I think she does not want to risk taking away my coping mechanism (however detrimental that may be). And also, the medication I am asking for is bloody expensive (I checked in the BNF)
So I am left with nothing, or a two year wait. Or worse. I am left with open wounds. Practically encouraged to continue with the unhelpful coping mechanisms. I am trying to engage with the charity sector now. I am trying not to give up.
What is left now? The prospect of debt. Overseas prescriptions. Unscrupulous private companies.
Or acceptance. The acceptance that despite working for the NHS, despite fighting for the NHS, I will not get the help that I so desperately need. That I was ready to put the effort in for. That parity of esteem is simply a myth.
I will either chose to continue life as it is. Or I will choose not to. What will happen when I move to the acceptance stage is probably what frightens me most. It could mean losing my career. It could mean losing my life.
The most absurd thing, is I am even starting to wonder if it is better that the NHS is for sale. Because it (or the trust in which I live and previously worked for) has failed me. Or that is how it feels. Every time I see the slogan for the current campaign it hurts a little more. I feel I am inadequate as it is. I see this and I think, if every mind matters then why doesn't mine?
I will either chose to continue life as it is. Or I will choose not to. What will happen when I move to the acceptance stage is probably what frightens me most. It could mean losing my career. It could mean losing my life.
The most absurd thing, is I am even starting to wonder if it is better that the NHS is for sale. Because it (or the trust in which I live and previously worked for) has failed me. Or that is how it feels. Every time I see the slogan for the current campaign it hurts a little more. I feel I am inadequate as it is. I see this and I think, if every mind matters then why doesn't mine?
In January, I wanted to get well. I still want to get well. But it's almost January again. I am more harmed, feel more traumatised by my experiences this year, I have put myself through the pain of retelling parts of my story that remained shut away for many many years. I have been broken. I have been told that I have a disordered personality, which is a difficult diagnosis to carry in it's self. I struggle not to take it personally. Not to feel like a victim. It is harder knowing that I will not be offered the support to heal. I am grieving all over again. For what I have lost, but also for all that I could be. I just don't know if I can do it for much longer any more.
And if I don't, please don't say I didn't try.
P.S I don't work in the same trust that I am a 'patient' in .
P.S I don't work in the same trust that I am a 'patient' in .
Comments
Post a Comment